Written by Michelle Champlin BSc Pod., M.Ch.S., S.R., Ch., (UK)
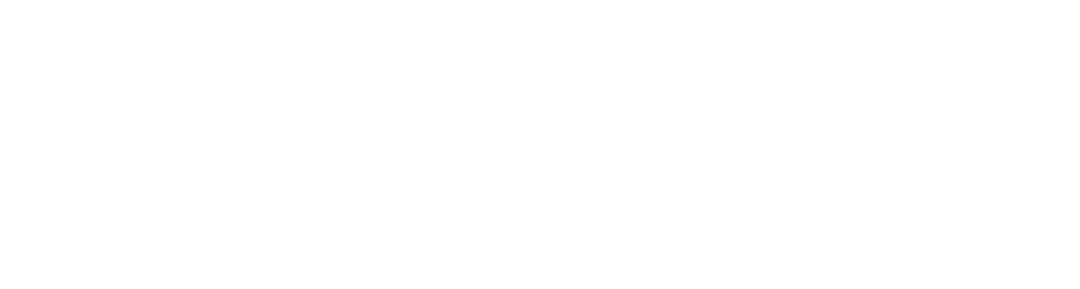
‘Onychocryptosis’ is a medical term for an ingrown toenail. It occurs when part of the nail penetrates or increases pressure on the skin which causes pain, inflammation, hyper-granulated tissue and sometimes even bacterial infection in the soft tissue around the toenail.
Why do I get ingrown toenails (and they keep coming back)?
The many causes of developing painful ingrowing toenails including:
Incorrect cutting of the nail (too short / leaving sharp edges / cutting down the sides of the toenail)
An underlying biomechanical issue of the foot such as ‘Pronation’ of the hallux – where the toe rotates – and Hallux Valgus (bunions) causing skin to bulge on one side of the nail leading to an increase in pressure between of the toenail on the surrounding toe
Involuted nails – where the nail is growing extremely curved at one or both edges rather than lying straight across the nail bed
Tight shoes causing increased pressure on the nail and skin
Trauma – deforming the nail growth will increase the chances of developing into an ingrown nail, such as kicking something or dropping an object on your toe
Swollen toes – chubby digits or due to swelling during pregnancy can increase the skin bulging around the nail leading to an ingrown nail
Fungal nail infections - deformed, brittle or thickened nails increase the chances of developing an ingrown nail.
How can a Podiatrist help?
At Dubai Podiatry Centre, we work differently to Chiropodists and even other Podiatrists. We recommend treating any underlying root cause of all problems, so that the problem doesn’t come back. Rather than constantly seeing a podiatrist to correctively trim back your nail (which tends to keep coming back as the underlying problem hasn’t been fixed), we advise finding out and fixing any root cause. For example, if the ingrowing nail is due to an internally rotated toe and over-pronation at the ankle, simply correctively cutting the nail will not fix the issue for more than a few weeks. We may advise corrective orthotics to re-align your foot and ankle correctly to stop the resulting pressure on the toe and nail. Otherwise, you may find yourself constantly treating the painful ingrowing nail, which may simply be a symptom of an underlying biomechanical issue.
Other issues such as an underlying chronic fungal nail infection should also be treated and addressed, as otherwise your nail will continue to grow in thickened / ingrown.
Therefore, we look at every single factor from your footwear, to hormones, underlying bacterial and/or fungal infections, growth pattern of the nail, biomechanics of your foot, ankle and leg and general medical history to get to the cause of why your nail is ingrowing. Then, you can be sure that you are receiving the correct specialist nail advice and precise course of treatment appropriate to the cause of your ingrowing nail. At Dubai Podiatry Centre, it is an important part of our ethos that patients are fully informed and can make treatment decisions based on a full assessment and best course of action for both the short and long term.
Diabetes and Ingrowing Nails
If you are Diabetic, it is also very important that you see a Podiatrist at least annually for your regular foot check up. If you experience any foot issue, including early signs of an ingrowing nail, seek prompt and early treatment from your Podiatrist to prevent more serious complications.
What should I do if I have an ingrowing nail?
We treat every nail as if it were our own, and know how painful ingrowing nails are. For permanent help and treatment of your painful ingrowing nail, come and see the nail experts at Dubai Podiatry Centre. Chief Podiatrist Michelle Champlin advises early intervention and rather than just constantly trimming the nail and putting up with pain every month, identify and fix any underlying cause.
Do not ever cut down the sides of your nail, or let anyone except a qualified medical professional such as a Podiatrist, do this. Do not let a pedicurist cut down the sides of your nail. Before seeing your Podiatrist, you can soak the feet for 10-15 minutes in a warm saline solution. Do not oversoak and keep the toe clean and dry otherwise. Avoid tight fitting hosiery, socks and shoes. You can also pack a little piece of gauze or cotton under the side of the nail to lift the nail up from pressing into your skin, if you can. Make an appointment with your Podiatrist to stop the ingrowing nail from causing infection to the surrounding tissue and to stop the nail from ingrowing again. If you already see redness and pus, you should see your GP in the meantime for a course of antibiotics.
For caring and professional treatment for any toenail, foot or leg issue, contact Dubai Podiatry Centre on 04 3435390.
أظافر نام وتشفير الأظافر
بقلم ميشيل شامبلين
“”Onychocryptosis”” هو مصطلح طبي يشير إلى ظفر القدم الناشب. ويحدث ذلك عندما يخترق جزء من الظفر الجلد أو يزيد الضغط عليه مما يسبب الألم والالتهاب والأنسجة المفرطة الحبيبات وأحيانًا حتى العدوى البكتيرية في الأنسجة الرخوة حول ظفر القدم.
لماذا أحصل على أظافر نام (ويستمرون في العودة)؟
هناك العديد من الأسباب التي تؤدي إلى ظهور أظافر مؤلمة في أصابع القدم، بما في ذلك:
قطع غير صحيح للظفر (قصير جدًا / ترك حواف حادة / قطع جوانب ظفر القدم)
مشكلة ميكانيكية حيوية أساسية للقدم مثل “كب” إبهام القدم – حيث يدور إصبع القدم – وإبهام القدم الأروح (الأورام) ” مما يتسبب في “انتفاخ” الجلد على جانب واحد من الظفر مما يؤدي إلى زيادة الضغط بين من الظفر على اصبع القدم المحيطة بها
الأظافر الملتفة – حيث ينمو الظفر منحنيًا للغاية عند إحدى الحافتين أو كلتيهما بدلاً من الاستلقاء بشكل مستقيم عبر سرير الظفر
الأحذية الضيقة تسبب زيادة الضغط على الظفر والجلد
الصدمة – يؤدي تشوه نمو الظفر إلى زيادة فرص التطور إلى ظفر نام، مثل ركل شيء ما أو إسقاط جسم على إصبع قدمك.
تورم أصابع القدم – يمكن أن تؤدي الأصابع السمينة أو بسبب التورم أثناء الحمل إلى زيادة انتفاخ الجلد حول الظفر مما يؤدي إلى ظهور ظفر نام
التهابات الأظافر الفطرية – الأظافر المشوهة أو الهشة أو السميكة تزيد من فرص الإصابة بالظفر الناشب.
كيف يمكن لطبيب الأقدام المساعدة؟
في مركز دبي لعلاج الأقدام، نعمل بشكل مختلف عن أطباء تقويم الأقدام وحتى أطباء الأقدام الآخرين. نوصي بمعالجة أي سبب جذري أساسي لجميع المشاكل، حتى لا تعود المشكلة مرة أخرى. بدلاً من رؤية طبيب الأقدام باستمرار لقص ظفرك بشكل تصحيحي (والذي يميل إلى العودة مرة أخرى لأن المشكلة الأساسية لم يتم حلها)، ننصحك بمعرفة أي سبب جذري وإصلاحه. على سبيل المثال، إذا كان الظفر الناشب ناتجًا عن استدارة إصبع القدم للداخل وزيادة في الكب في الكاحل، فإن مجرد قطع الظفر بشكل تصحيحي لن يحل المشكلة لأكثر من بضعة أسابيع. قد ننصح باستخدام أجهزة تقويم العظام التصحيحية لإعادة محاذاة قدمك وكاحلك بشكل صحيح لوقف الضغط الناتج على إصبع القدم والأظافر. بخلاف ذلك، قد تجد نفسك تعالج باستمرار الظفر المؤلم، والذي قد يكون ببساطة أحد أعراض مشكلة ميكانيكية حيوية كامنة.
يجب أيضًا معالجة المشكلات الأخرى مثل عدوى الأظافر الفطرية المزمنة الكامنة ومعالجتها، وإلا فسيستمر ظفرك في النمو بشكل سميك أو نام.
لذلك، نحن ننظر إلى كل عامل من حذائك، إلى الهرمونات، والالتهابات البكتيرية و/أو الفطرية الكامنة، ونمط نمو الظفر، والميكانيكا الحيوية للقدم والكاحل والساق والتاريخ الطبي العام للوصول إلى سبب سبب ظفرك. هو نام. بعد ذلك، يمكنك التأكد من أنك تتلقى المشورة المتخصصة الصحيحة للأظافر ودورة العلاج الدقيقة المناسبة لسبب نمو الظفر لديك. في مركز دبي لعلاج الأرجل، يعد جزءًا مهمًا من أخلاقنا أن يكون المرضى على علم تام ويمكنهم اتخاذ قرارات العلاج بناءً على تقييم كامل وأفضل مسار للعمل على المدى القصير والطويل.
مرض السكري ونمو الأظافر
إذا كنت مصابًا بمرض السكري، فمن المهم جدًا أيضًا أن ترى طبيب الأقدام سنويًا على الأقل لإجراء فحص منتظم لقدمك. إذا واجهت أي مشكلة في القدم، بما في ذلك العلامات المبكرة لظفر نام، فاطلب العلاج الفوري والمبكر من طبيب الأقدام الخاص بك لمنع حدوث مضاعفات أكثر خطورة.
ماذا علي أن أفعل إذا كان لدي ظفر نام؟
نحن نتعامل مع كل ظفر كما لو كان خاصًا بنا، ونعلم مدى الألم الذي يسببه نمو الأظافر. للحصول على مساعدة دائمة وعلاج للظفر الناشب المؤلم، تفضل بزيارة خبراء الأظافر في مركز دبي لعلاج الأرجل. تنصح رئيسة أطباء الأقدام ميشيل شامبلين بالتدخل المبكر، وبدلاً من مجرد تقليم الظفر باستمرار وتحمل الألم كل شهر، يجب تحديد السبب الكامن وإصلاحه.
لا تقم أبدًا بقص جوانب ظفرك، أو تسمح لأي شخص باستثناء أخصائي طبي مؤهل مثل طبيب الأقدام، بالقيام بذلك. لا تدع أخصائي العناية بالأقدام يقطع جوانب ظفرك. قبل زيارة طبيب الأقدام، يمكنك نقع القدمين لمدة ١٠-١٥ دقيقة في محلول ملحي دافئ. لا تبالغ في نقع القدم وحافظ على إصبع القدم نظيفًا وجافًا. تجنب الجوارب والجوارب والأحذية الضيقة. يمكنك أيضًا وضع قطعة صغيرة من الشاش أو القطن أسفل جانب الظفر لرفع الظفر عن الضغط على جلدك، إذا استطعت. حدد موعدًا مع طبيب الأقدام الخاص بك لمنع الظفر الناشب من التسبب في العدوى للأنسجة المحيطة ولمنع نمو الظفر مرة أخرى. إذا رأيت بالفعل احمرارًا وصديدًا، فيجب عليك مراجعة طبيبك العمومي في هذه الأثناء للحصول على دورة من المضادات الحيوية.
للحصول على رعاية وعلاج احترافي لأي مشكلة في أظافر القدم أو القدم أو الساق، اتصل بمركز دبي لعلاج الأقدام على الرقم ٠٤٣٤٣٥٣٩٠.


 People with Diabetes should pay extra special care to their feet.
Those who lead a healthy lifestyle with well controlled Diabetes and get annual feet checks should continue to have fantastic trouble free feet.
Those who have untreated diabetes or live a poor lifestyle are more likely to develop complications which include blindness, kidney and heart disease, stroke and loss of limbs.
Diabetes often leads to poor blood circulation. This decreases the circulation getting to the legs and feet which can cause injuries in the feet to heal poorly and can create ulcers, changes in shape of the feet, and loss of feeling.
Diabetes and the UAE Facts:
Prevalance of Diabetes among citizens of the UAE is second highest in the world
20% of UAE Residents have Diabetes
25% of Emirati Nationals have Diabetes
Up to 90% of people with Type 2 Diabetes were shown to be triggered by lifestyle factors, like poor diet and limited exercise
Diabetes = poor blood circulation Decreased circulation getting to the legs & feet
Reduces the amount of Oxygen Injuries to heal poorly/slowly
and Nutrition getting to the skin Ulcers & Infections
& tissues
Swelling & Dryness of the feet
Treatment and Prevention
Have an annual Pain Free Diabetic Assessment of your feet with your Podiatrist. Here we check the circulation and sensation of your feet.
Wear cushioned, supportive footwear
Check your feet Daily for cuts, sores and hard skin “ Use a mirror if needed
Wear shoes and socks at all times to limit chances of ˜friction sores™
Dry between your toes
Do NOT use corn pads or attempt self removal of hard skin “ see a Podiatrist
Control your Diabetes
Make healthy lifestyle choices with Diet and Exercise
Keep your blood sugar levels normal
Stop Smoking
Work with your GP to create a plan that fits you
People with Diabetes should pay extra special care to their feet.
Those who lead a healthy lifestyle with well controlled Diabetes and get annual feet checks should continue to have fantastic trouble free feet.
Those who have untreated diabetes or live a poor lifestyle are more likely to develop complications which include blindness, kidney and heart disease, stroke and loss of limbs.
Diabetes often leads to poor blood circulation. This decreases the circulation getting to the legs and feet which can cause injuries in the feet to heal poorly and can create ulcers, changes in shape of the feet, and loss of feeling.
Diabetes and the UAE Facts:
Prevalance of Diabetes among citizens of the UAE is second highest in the world
20% of UAE Residents have Diabetes
25% of Emirati Nationals have Diabetes
Up to 90% of people with Type 2 Diabetes were shown to be triggered by lifestyle factors, like poor diet and limited exercise
Diabetes = poor blood circulation Decreased circulation getting to the legs & feet
Reduces the amount of Oxygen Injuries to heal poorly/slowly
and Nutrition getting to the skin Ulcers & Infections
& tissues
Swelling & Dryness of the feet
Treatment and Prevention
Have an annual Pain Free Diabetic Assessment of your feet with your Podiatrist. Here we check the circulation and sensation of your feet.
Wear cushioned, supportive footwear
Check your feet Daily for cuts, sores and hard skin “ Use a mirror if needed
Wear shoes and socks at all times to limit chances of ˜friction sores™
Dry between your toes
Do NOT use corn pads or attempt self removal of hard skin “ see a Podiatrist
Control your Diabetes
Make healthy lifestyle choices with Diet and Exercise
Keep your blood sugar levels normal
Stop Smoking
Work with your GP to create a plan that fits you Get Arches in Your Feet
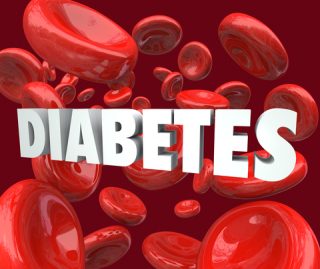
The Medial Longitudinal Arch (MLA) extends from the inside of your heel along the bottom of your foot and connects to the big toe. It is a critical structure to allow for good shock absorption of the forces transmitted through the body from the feet during gait.
When the MLA is lower to the ground or ˜flat™ it can cause an uncontrolled over pronation of the ankle joint.
Overpronation is where the ankle joint ˜rolls in.™ Common injuries that occur from a flat MLA and over pronation include: Achilles tendonitis, heel pain, bunions, stress fractures, arch pain, shin splints and over use tendon injuries.
Custom made Orthoses Devices can be implemented to strengthen the MLA and maintain a neutral ankle joint alignment to control over pronation and relieve pain.
A custom made Orthoses is made by taking a mould of your feet to get the exact shape of each foot. It is then uniquely modified to create the individual™s perfect Medial Longitudinal Arch and neutral ankle joint to allow the ideal heel to toe gait.
Get Arches in Your Feet
The Medial Longitudinal Arch (MLA) extends from the inside of your heel along the bottom of your foot and connects to the big toe. It is a critical structure to allow for good shock absorption of the forces transmitted through the body from the feet during gait.
When the MLA is lower to the ground or ˜flat™ it can cause an uncontrolled over pronation of the ankle joint.
Overpronation is where the ankle joint ˜rolls in.™ Common injuries that occur from a flat MLA and over pronation include: Achilles tendonitis, heel pain, bunions, stress fractures, arch pain, shin splints and over use tendon injuries.
Custom made Orthoses Devices can be implemented to strengthen the MLA and maintain a neutral ankle joint alignment to control over pronation and relieve pain.
A custom made Orthoses is made by taking a mould of your feet to get the exact shape of each foot. It is then uniquely modified to create the individual™s perfect Medial Longitudinal Arch and neutral ankle joint to allow the ideal heel to toe gait.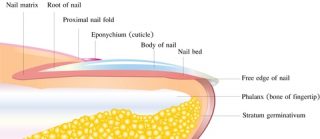 Flatten your Curved Nails
Curved nails are where one or both of the linear aspects of a nail starts to form down into the skin to form a curved shape.
Having curved nails is a common problem and can cause great distress to the surrounding skin which can lead to pain, inflammation and even infections.
To correct the curvature and pain it is important to address how the curves developed. Nails can curve due from certain medications, ageing, tight footwear, hereditary, improper cutting, fungal infections and skin problems such as Psoriasis or Ecemza.
Treatment involves assessing the steepness of the curve and choosing the best treatment plan for each patient.
Options include
Corrective Nail Trimming
Nail Braces: where a small plastic device is medically applied to the top of the curved nail. The brace works with a spring-like action to pull up the corners of the curve to straighten out the nail. Leaving a pain free, perfect toe nail. Treatment period = 6-8wks.
Partial Nail Avulsion (PNA): If the curve or nail rydge is steep then a PNA may be recommended. A simple procedure where local anasethetic is administered to the side of the nail to achieve anasethsia. The small section of aggravating nail is then carefully removed right from the nail root. This procedure takes approximately one hour and usually ready to exercise and swim within 10days.
Flatten your Curved Nails
Curved nails are where one or both of the linear aspects of a nail starts to form down into the skin to form a curved shape.
Having curved nails is a common problem and can cause great distress to the surrounding skin which can lead to pain, inflammation and even infections.
To correct the curvature and pain it is important to address how the curves developed. Nails can curve due from certain medications, ageing, tight footwear, hereditary, improper cutting, fungal infections and skin problems such as Psoriasis or Ecemza.
Treatment involves assessing the steepness of the curve and choosing the best treatment plan for each patient.
Options include
Corrective Nail Trimming
Nail Braces: where a small plastic device is medically applied to the top of the curved nail. The brace works with a spring-like action to pull up the corners of the curve to straighten out the nail. Leaving a pain free, perfect toe nail. Treatment period = 6-8wks.
Partial Nail Avulsion (PNA): If the curve or nail rydge is steep then a PNA may be recommended. A simple procedure where local anasethetic is administered to the side of the nail to achieve anasethsia. The small section of aggravating nail is then carefully removed right from the nail root. This procedure takes approximately one hour and usually ready to exercise and swim within 10days.